The Pathophysiology of Obstructive Sleep Apnea

A discussion of the pathophysiology, risk factors, diagnosis, and treatment of obstructive sleep apnea.
Pathophysiology
Pathophysiology is the medical term used to describe the process of why things go wrong. So, what is obstructive sleep apnea? It is the process of stopping breathing due to an obstruction. If you were to look at a cross section of the head of a person, there are two areas where the air can travel. It can go into the nose and it can go into the mouth.
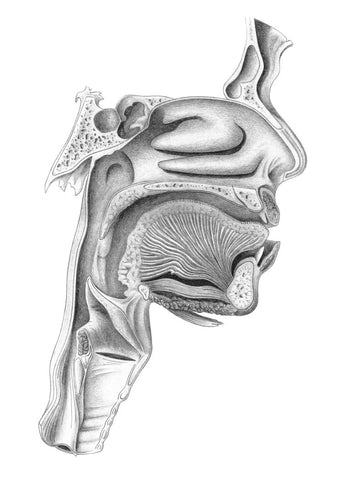
The problem is in the area where fat is stored in the back of the tongue. There can be an obstruction in that area due to fat storage. So, typically, what will happen is that when you are awake, you can breathe without problem.
You fall asleep, your muscles relax, and when your muscles relax, they become flexible. This airway is not like a plastic pipe; it is not rigid. And especially with gravity and lying on your back, your tongue muscle can fall back, and this area becomes loose, and finally it can become obstructed.
The diaphragm is contracting, causing the lungs to expand. Thus, you have a negative pressure that will try to induct air. But because this pathway is blocked, there will not be any airflow, there is a blockage of airflow. That is the pathophysiology of obstructive sleep apnea.
Patterns of oxygen saturation when sleeping
Because the medulla oblongata of the brain sends signals to the lungs, they breathe on their own while you sleep. However, no air can enter through the closed channel in the back of the neck. As a result of the lack of air, your pulse oximetry, O2 saturation, begins to diminish.
As a result, the brain receives a signal that something is wrong. As a result, the brain wakes up from its slumber, sometimes completely. The brain then sends a signal to that part of the body to tighten up and the air begins to flow again. The sympathetic response from the lungs is stopped, air begins to flow again, and the brain goes to sleep. The area in the back of the throat becomes flabby and closes once more.
REM sleep is the next condition that can aggravate the condition. REM is an acronym for rapid eye movement. You dream when you are in a state of REM sleep mode. As a result, your body has a protection mechanism that causes you to become paralyzed. You would act out your dreams if you were not paralyzed. As a result, most of your muscles are paralyzed. Muscles that try to keep your airways open are included in this. So, until the patient is in a position where there is no sleep apnea or the patient falls into a different form of sleep, you will get this type of wavy oxygen pattern.
Supine Sleeping Position
Sleeping in a supine position is the first major risk factor for sleep apnea. Anything that worsens blockage will exacerbate sleep apnea. The supine sleeping posture does not cause sleep apnea in all patients, but can exacerbate it in others. The tongue can fall back and obstruct the passageway. As a result, sleeping in a supine position is a key factor.
REM Sleep
The next condition that can exacerbate the condition is sleep in the REM state. REM stands for Rapid Eye Movement. When you are in a state of REM Sleep, you are dreaming. And because of that, the body has a defense mechanism where you become paralyzed. If you were not paralyzed, you would act out your dreams. Therefore, most of the muscles in your body are paralyzed. Included are the muscles that try to keep your airway open.
What are the risk factors for the diagnosis of obstructive sleep apnea (OSA)?
What are the factors that make this condition more likely? One of the main ones is the fact that you are male. Men tend to store more fat in the neck. This does not mean that women cannot have it. For men, in terms of the prevalence of stopping breathing, not necessarily having the syndrome of sleep apnea, but just stopping breathing at night, more than five times per hour, 24% of men do that.
For women, it is 9% who stop breathing more than five times per hour at night, again not necessarily due to obstructive sleep apnea. The prevalence of actual sleep apnea, patients who stopped breathing more than five times per hour and, in addition, have excessive daytime sleepiness, because they do not get good sleep at night, because they keep getting aroused, then it drops to about 4% for men and 2% for women.
What is the prevalence of obstructive sleep apnea in the general population? It is about on average about 3%. The incidence will be much higher for a clinic population or a hospital population.
Obstructive Sleep Apnea and Menopause
Although the prevalence for women is lower, they catch up with men after menopause and after the age of 40 to 55, women catch up completely with men in terms of their risks.
Obstructive Sleep Apnea and Obesity
People often think that only obese people get obstructive sleep apnea. This is not the case, but it is a significant risk factor. If you have obesity, it increases your risk of sleep apnea about 10 to 14 times. Just a 10% increase in weight can result in a six-fold increase over four years.
Obstructive Sleep Apnea and Race
OSA is more than twice as prevalent in black people than in white people. People in this community with OSA also experience significantly higher rates of obesity and high blood pressure. Black women develop OSA at a much younger age and black men experience more dangerous drops in blood oxygen than their white counterparts.
Research also shows that Asians are also more likely than their white peers to suffer OSA. Obesity is not necessarily a key factor, as is often assumed. Sometimes bone structure can factor into breathing problems during sleep.
A study in 2000 showed that most East Asian men with severe OSA had a normal body mass index measure due to facial structures that contribute to breathing disturbances.
Obstructive Sleep Apnea and Genetic Factors
If you have a first degree relative with OSA, that increases your risk of OSA from 22% to about 86%. That is a huge increase. First-degree relatives are mothers, fathers, brothers, sisters.
Obstructive Sleep Apnea and Age

The final main risk factor for OSA is age. If you look at the graph, it goes up with age until it reaches about 50 or 60, it then stabilizes until 70, and then increases again.
Age-related conditions that can increase it are conditions such as acromegaly. Testosterone treatment can make it worse. Hypothyroidism is not an indication of OSA.
Finally, menopause. It is like the equalizer for women, after the onset of menopause, the susceptibility for women of OSA becomes the same as for men.


Leave a comment